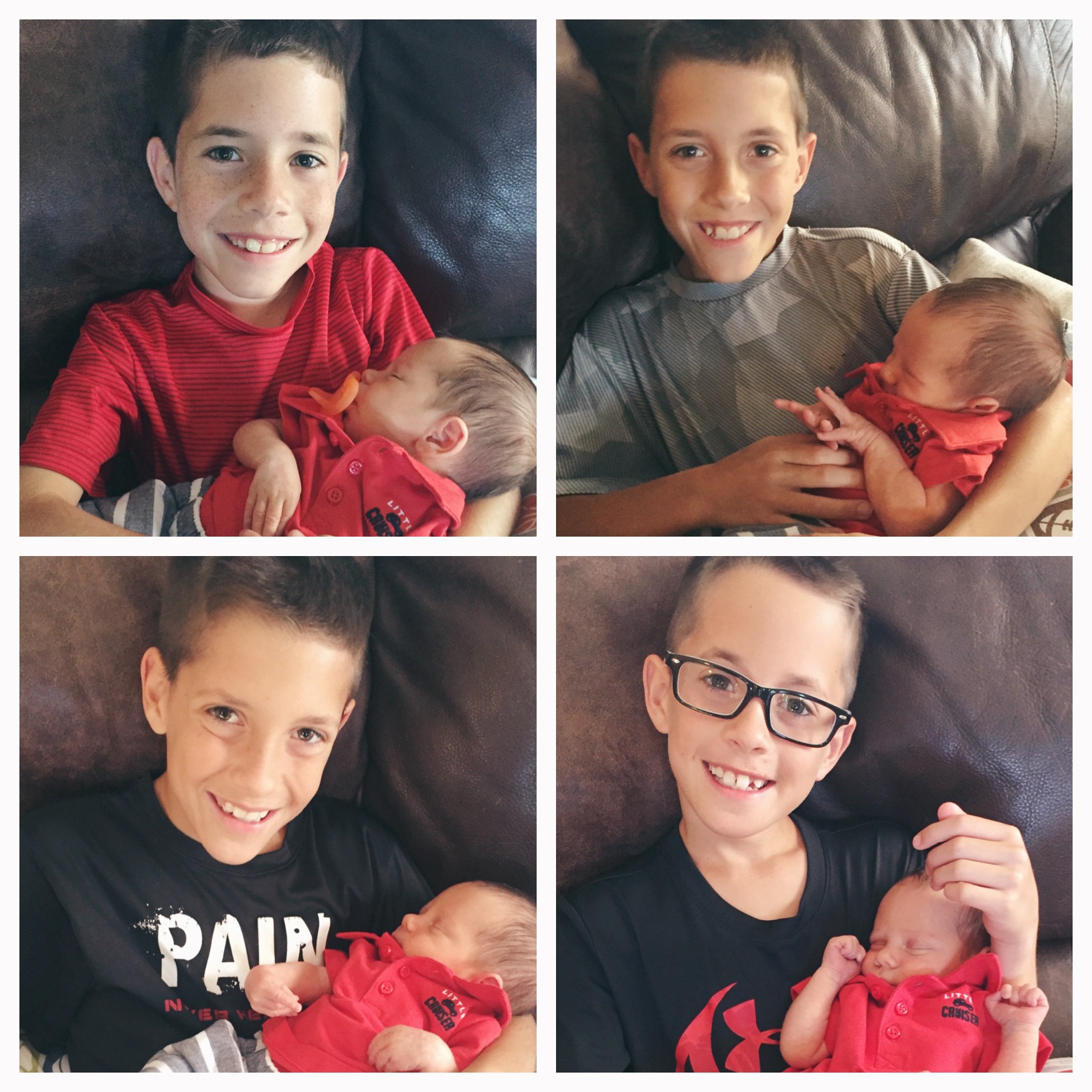
Six Months of Hudson Bradley

I can’t believe we are 6 months into Hudson’s life. This 1/2 a year has FLOWN! What a gift each day has been with this little guy! I’m starting to see the little boy coming out in this baby, which is equally exciting to see him grow, and sad that his baby days are numbered. Milestones …
Read More